Kent Community Health NHS Foundation Trust (KCHFT) wanted to support staff at care homes in Kent in order to help them monitor their residents more effectively, reduce the number of GP call outs and reduce the stress for residents associated with having to go to hospital. The team deployed the DOC@HOME® remote monitoring system from Docobo across two care homes.
KCHFT Project Manager Andy Platt says
Together with the excellent results we have achieved, it’s also important to realise how using this is benefiting care home residents. Their health is being closely monitored and any deterioration in their health is detected much quicker than before, resulting in spending less time with GPs and in hospital and more time feeling comfortable in their homes. A visit to A&E can be stressful and unsettling.
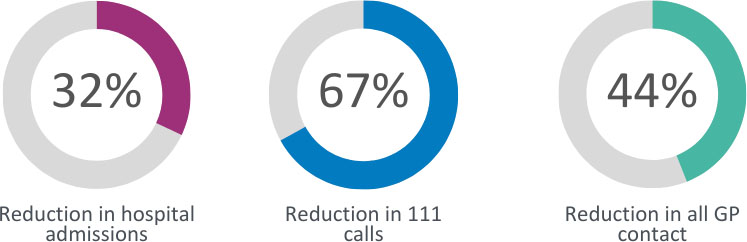
Key results
The project has produced impressive results across the two care homes:
The project has benefitted care home staff, residents and clinicians alike.
Background
The team at KCHFT decided to use the DOC@HOME remote monitoring solution to monitor residents, so that care home teams could carry out simple health checks with residents and recorded these via the DOCOBOAPP™ , then send these to the Complex Care Team.
Docobo supports healthcare providers enabling them to monitor their elderly, unwell and frail patients in their own homes or care homes, by providing DOC@HOME, a proven UK developed, IG compliant, remote monitoring solution. DOC@HOME works on either a patient’s own device or on an easy to use CAREPORTAL and allows clinical staff to remotely monitor their patients. It also allows people to monitor patients with longterm conditions, such as heart failure, diabetes and chronic obstructive pulmonary disease (COPD).
How did it work?
The telehealth project was initially piloted for six months in two care homes in Maidstone, Kent. Using a telehealth solution, staff at the care homes carried out simple health checks with residents each day and recorded these via the DOCOBOAPP. These could be simple healthcare checks asking condition-specific questions, such as: had they felt dizzy, short of breath or more tired than normal. Care home staff recorded this information on a tablet and it was then closely monitored by the Complex Care Team at KCHFT, who looked at the data trends and were able to detect if a resident’s health was deteriorating.
The team set up parameters for each patient and if their observations fell outside of these, an alert was sent to the on duty Complex Care nurse who would then respond to the alert. The team could then immediately step in with the most appropriate action, which might be as simple as carrying out increased observations to monitor a patient more closely or tweaking a patient’s medication.
KCHFT Project Manager Andy Platt says:
Care homes tend to be very high users of NHS services in general and usually have a number of residents with a lot of complex health issues. These patients aren’t monitored very closely and usually only receive care once the care home staff notices that the patient’s health has visibly deteriorated – at this point they would call a GP, 111 or 999. Having a Complex Care nurse monitoring their health daily reduces the possibility of an avoidable visit to A&E. We were aiming to reduce hospital admissions, calls to 999 and GP visits, each by 10 per cent, but we were delighted to far surpass this initial target.









